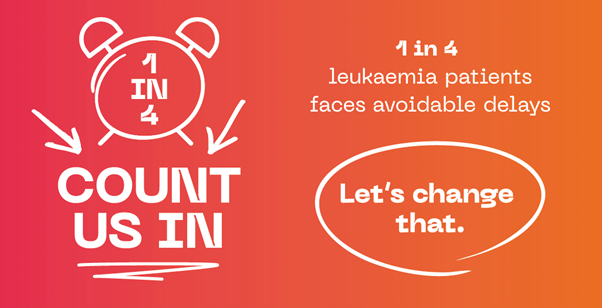
This shocking statistic comes from our new campaign, Count Us In, which highlights the extent of missed opportunities in diagnosing leukaemia earlier.
For many people with leukaemia, the warning signs were there, but they weren’t diagnosed in time. Often all this takes is a simple full blood count test.
“I saw my GP several times over months with symptoms including bone pain, exhaustion, bruising and mouth ulcers. I wasn’t offered a full blood count test and was told it was rheumatoid arthritis, but the medication didn’t help. It wasn’t until I fainted and ended up in A&E four months later that I was finally diagnosed with AML. While the care I received was exceptional and I feel very lucky to be in remission, that is not the case for everyone with leukaemia. I fully support Leukaemia UK’s call for change, early diagnosis saves lives.”Tracey Palmer-Hole, AML survivor
The current system is missing too many people, too often. It’s time to improve GP referral pathways, increase blood test access, and make earlier diagnosis the norm.
This is why we are calling for the Government to use the upcoming National Cancer Plan to commit to stopping avoidable delays in leukaemia diagnosis.
In our new report, we have set out clear, actionable recommendations to ensure patients are diagnosed as early as possible, giving them the best chance of survival.
Disclaimer: This work was supported in part with funding from AbbVie, J&J and Novartis. These organisations had no input into the development, design, delivery or interpretation of the evidence, and no editorial input into this report.